The Wrong Pipe: Aspiration’s final destination
With help from Ed Bice, M.Ed., CCC-SLP
You are doing a clinical assessment on a patient. You give her a cup filled with 3 oz of water and ask her to drink it without stopping. She proceeds, but begins coughing violently halfway through the trial… Uh oh. This patient definitely aspirated. But what does it mean? What do I do from here? Will the patient get pneumonia? Will she be OK??
Passing the Golden Vocal Fold Gates
The Answer? Well, it depends (You were probably expecting that response weren’t you?). Think about the way the respiratory system is structured first. It’s sort of like an upside down tree with the trachea as the trunk. As it descends, the branches go from larger to smaller from the mainstem bronchi to the tiny stems of the terminal bronchioles where the alveoli are. None of these tubes are as big as you might imagine in your head. The trachea is only about the width of the knuckle of your pinky finger. This width splits in half 23x making the terminal bronchioles minuscule and exponentially smaller than the trachea (1/100,000th the size of your pinky!). So these are very small tubes we are talking about here. And what happens when bigger things try to go through smaller tubes? They get stuck. But where?
Thicker viscosities and solids are more likely to obstruct the higher airways including the pharynx, larynx, and trachea (i.e. choking), and the mainstem bronchi (which would essentially suffocate an entire lung). Liquids on the other hand are by definition more fluid and more likely to #1 end up in the lower airways and #2 end up closer to the gravity dependent areas of the lungs (the tiny bronchioles) especially with large volume aspiration. Komiya et al., 2013 found that most aspirators developed bronchopneumonia (68%) vs lobar pneumonia (15%). As Ed Bice explained to me, we can think of smaller volumes of aspiration as a drop of water running down a wall. It’s not so much a stream from the ceiling to the floor, but a slow disbursement of fluid that lessens and spreads out as it makes it’s way down (think, chronic, trace aspiration). This may be why only a small percentage of individuals who aspirate thin liquids end up with pneumonia and/or respiratory compromise. The risk of aspiration and the impact of that aspiration are ultimately on a spectrum based on a myriad of factors. The event with the potential for the worst outcome though is choking...
Choking
Of course, choking is the biggest concern for dysphagia related complications as it is immediately life threatening. But what causes someone to be at a higher risk for choking? Research tells us that a patient is more likely to choke when she has few or no teeth, decreased salivary flow, and oral motor weakness. This is why we always first do an oral motor exam where we examine lingual and labial function, assess for xerostomia, and confirm adequate dentition (Yes, some may be able to chew without teeth, but a careful consideration of the costs and benefits should be considered with the interdisciplinary team to fully address the risk).
The type of food also matters. Larger pieces of harder, dryer consistencies are more likely to cause choking than smaller, softer, moister consistencies (no surprise there) with hot dogs causing more choking events than any other type of food. What came as a surprise to me was this study, which found that individuals without teeth were more likely to choke on soft/slick food.
Who should we be on the lookout for and what can we do? The risk of choking is increased in the elderly population (especially in those with cognitive deficits) so pay particularly close attention to those with advanced age. Hemsley et al., 2019 provides a great look at a comprehensive approach to reducing the risk of choking, which includes basic, but useful strategies such as keeping the patient in an upright posture, utilizing individualized safe feeding strategies, considering diet modification (if amenable to the patient as this may significantly decrease PO intake and quality of life), and maintaining adequate supervision.
Aspiration
The question isn’t just if the patient is aspirating, but what the patient is aspirating. In general, thicker consistencies with more contents, chemicals, and/or acid will be more harmful to the pulmonary tissues than thinner, clearer, less acidic substances. Think ice, water, and clear liquids vs coffee, soda, thick liquids, and solid matter. We don’t have a ton of research on the impact different types of material have on pulmonary health because these studies would be dangerous and irresponsible to conduct. BUT we DO know the more acidic a substance is, the more damage it causes to the pulmonary tissues. We know this because high acidic substances such as gastric contents may lead to a really nasty condition called aspiration pneumonitis. Further, this study on rabbits tells us that thickened liquids may be more harmful to the lungs than thin liquids. Overall, the thinner and lighter the material is, the easier it is to remove out of or diffuse into the pulmonary tissues. That’s right. Aspiration doesn’t mean those contents will be there forever. The lungs are quite good at responding to this invasion...
The Body’s Response
When aspiration occurs, our lungs don’t just sit there like two defenseless sacks; they engage their multiple levels of pulmonary defenses to clear out and fight off the intrusion. Tiny hairs line the airways and are covered with mucus so foreign materials get stuck and pulsate back up to the upper airway. Exhalation, the movement of the cilia, and our cough reflex should eliminate most of the foreign material so that it doesn’t obstruct the airway or cause an infection. Further, in utero (when essentially living under water), we develop aquaporins in our lungs, which are proteins that act as channels for thinner, lighter substances (like water) so they can diffuse into the blood stream instead of sticking around the respiratory system. Lastly, our body’s immune system has specialized white blood cells that are responsible for gobbling up and digesting potential infectious material before it escalates. If you want to read more about the lungs and keeping the lungs clean, check out my posts on the respiratory system and respiratory disease.
Quick note: After writing this, I recently came across this article by Palmer and Padilla which explains this process, if I’m being honest, much better than I just did and with wonderful diagrams. You can read the full text through the ASHA Wire, which I highly recommend.
Of course, these defenses may be compromised with disease processes, medical complexity, and certain risk factors. The development of aspiration pneumonia is not all about dysphagia, but instead is dependent on multiple factors as we know from Dr. Susan Langmore’s landmark study on the predictors of aspiration pneumonia as well as many follow-up studies on the topic which have reinforced and expanded her findings (for further reading on this topic check out this case study I did with Dr. James Coyle and Doreen Benson).
It’s become clear that small amounts of water may be relatively safe when introduced to the lungs through a relatively clean oropharynx without the harmful build up for oral pathogens. And as long as we are brushing our teeth before we go to bed then natural, silent, trace aspiration of secretions during sleep doesn’t appear to harm us (here is an updated look at this phenomena in people with sleep apnea). So the thinner and lighter the consistency the safer it is to the lungs. If we can keep the mouth clean, that’s better. And if we can control the volumes to just a small amount, even better! Even large amounts of thin liquid water can build up in lungs and begin to obstruct airflow and gas exchange. So what can we do to examine this risk and mitigate it on a case by case basis?
The Practical Part: What can we do to help?
What your patient is most likely to aspirate? Doing an instrumental study is the only way we can obtain this information. Once that’s done we can determine with increased accuracy what consistencies may end up in the lungs and how the patient might be able to prevent this from happening.
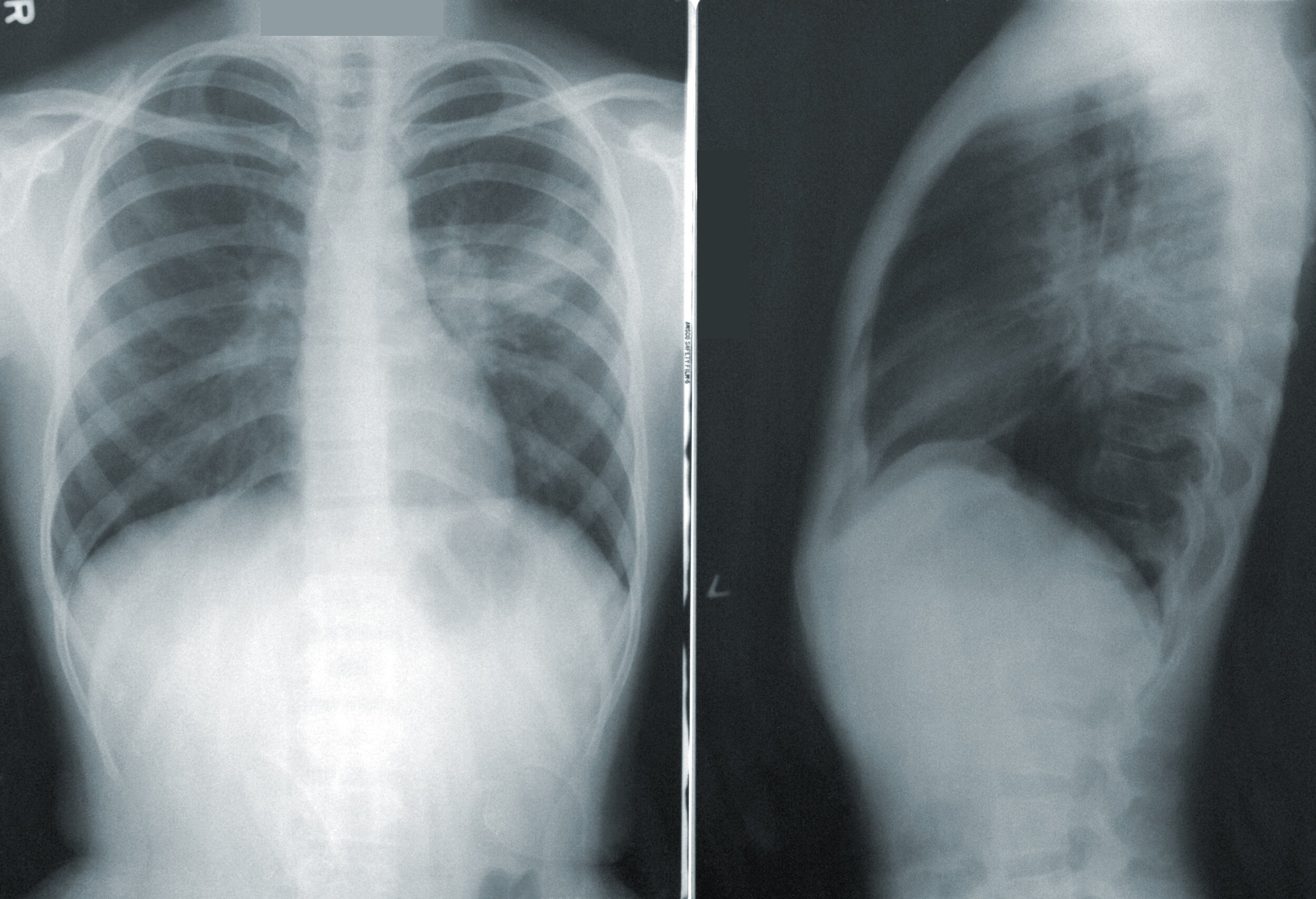
Look at chest imaging, the radiologist’s report, and discuss the findings with the attending physician and interdisciplinary team. Unfortunately, aspiration pneumonia is notoriously difficult to diagnose and is often misdiagnosed for that very reason. Mukhopadhyay and Katzenstein, 2007 studied food/particle aspiration in 59 patients and found that only 8.8% of the patients studied were correctly diagnosed with aspiration pneumonia. 22% of these patients were even misdiagnosed with a nepolasm. This study went on to show that all cases with aspiration presented with “infiltrates or nodules” which may give us some reason to dig deeper when we see these terms used for our patients. We can then work with the radiologist, pulmonologist, and physician team to determine if there is a possible obstruction or gravity dependent involvement and find out if that can be paired with dysphagia, a high risk for aspiration, signs of infection, and/or a change in respiratory status.
Remember, it’s not just if the patient is aspirating, it’s what that aspiration means for the patient and their overall status. People aspirate all the time, but pneumonia and respiratory issues only occur in a small percentage of those who have an unfortunate combination of health conditions. Determine which of these factors your patient has and if/how those factors can be mitigated.
And Discuss
Discussing our findings and the relevant factors with the patient could be the most important part of the management process. Being able to communicate what’s going on with your patient, what increases their probability of an adverse outcome, and how we can reduce that probability is what really provides value to your patient, their quality of life, and their well-being. It’s also the most fun part. When we get out of the dark office and into the bright patient room where we can use our emotions and empathy to truly understand and connect with the patient. And once we connect, then we can truly serve by finding what works best for them.
Liked this? Why not share it?
Leave a comment. I feed on feedback.